Abstract. The application of compensation strategies is an important element of gait rehabilitation in persons with Parkinson’s disease. While the efficacy of these strategies is generally very high, a tailored, personalized approach is necessary to determine the optimal strategies for every patient. We propose a straightforward, practical guide to the evaluation of compensation strategies in clinical practice: considering the primary gait target(s) to optimize functional mobility, the context in which the strategies will be employed in daily life, and patient-specific personal preferences. Furthermore, we introduce www.walkingwithparkinson.com as a resource on the available compensation strategies, developed specifically for persons with Parkinson’s disease, their carers, and (allied) healthcare professionals.
-
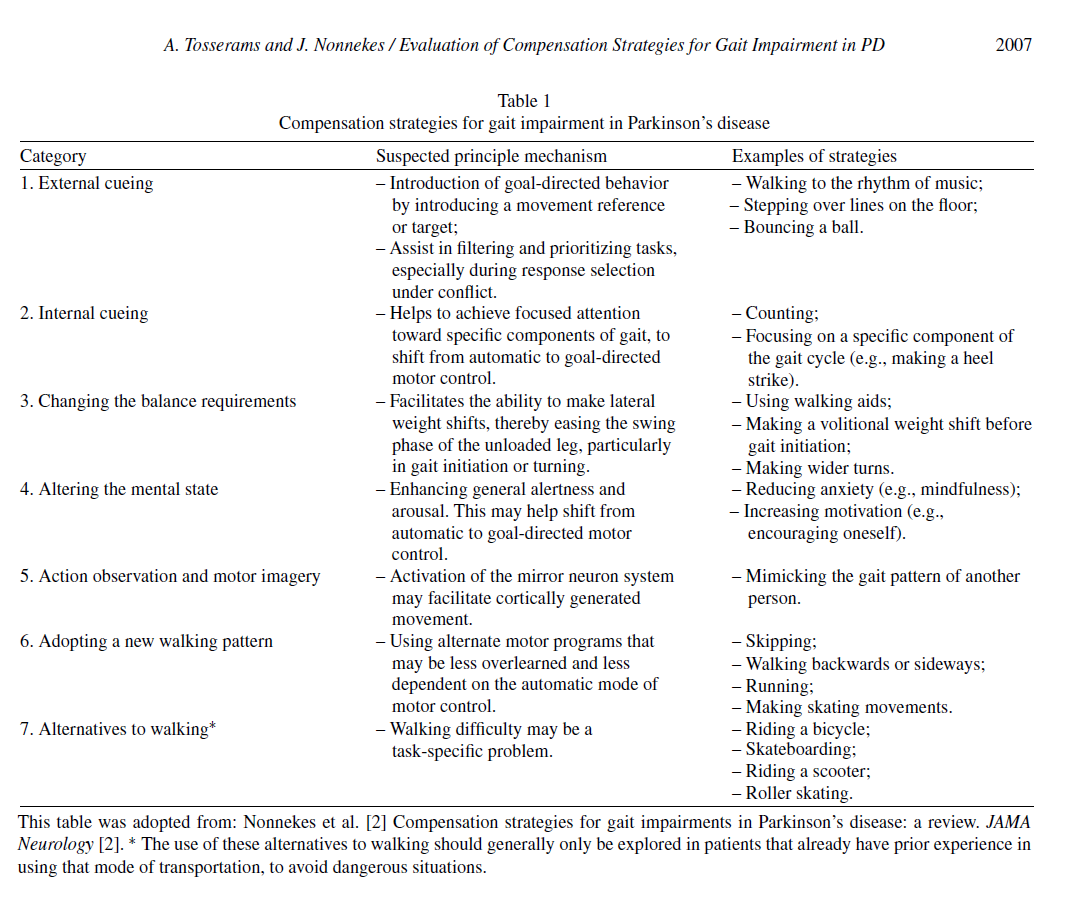
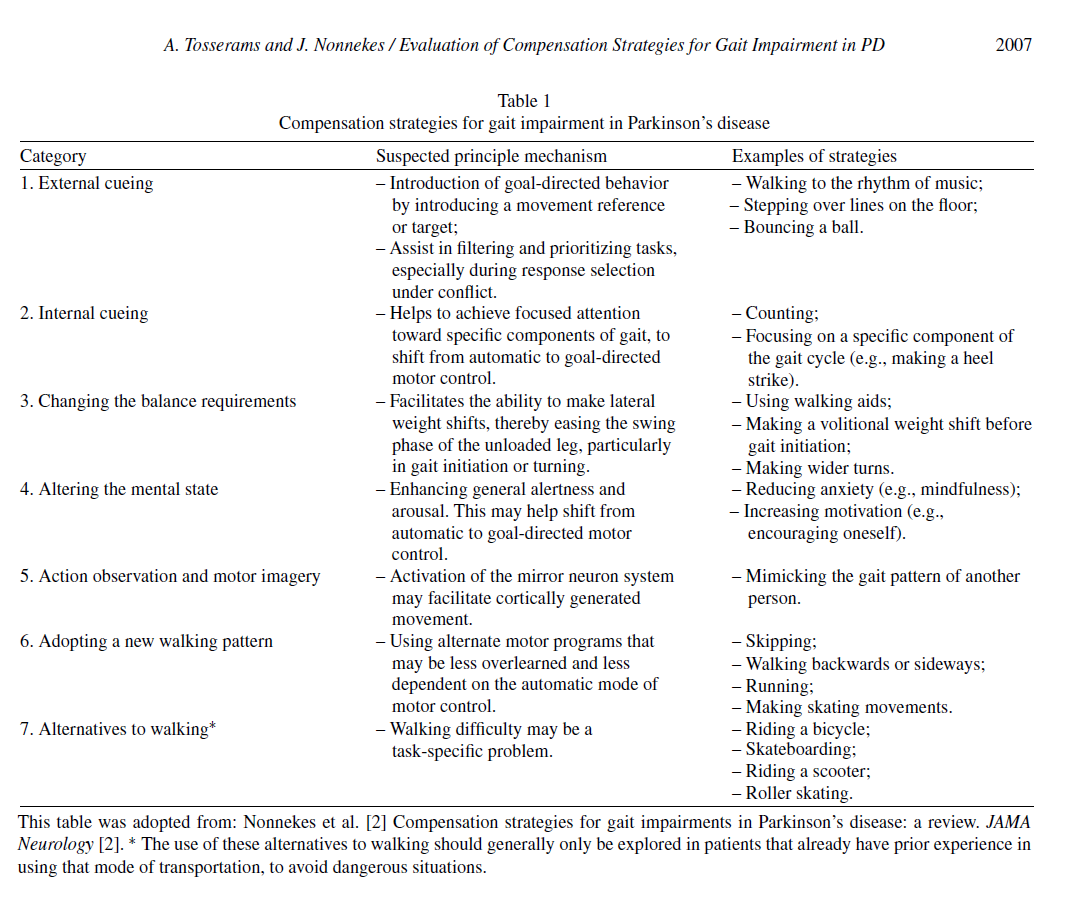
Gait impairments are among the most common and disabling symptoms of Parkinson’s disease (PD). Management consist of complementary pharmacological and non-pharmacological treatment options [1]. Physiotherapy is a cornerstone of the non-pharmacological pillar, and the application of compensation strategies is one of the elements of physiotherapy. These strategies comprise a wide range of ‘detours’ to improve walking capacity (Table 1) [2]. While the efficacy of gait compensation strategies is generally very high, the effects of specific strategies vary greatly between patients: what works spectacularly well in one patient, has no effect—or even aggravates gait impairment—in the next [3].
Therefore, a personalized approach to gait rehabilitation is imperative to find a suitable strategy for every person with PD and gait impairment. Ideally, every person with PD and gait impairment should be informed about compensation strategies by a healthcare provider (for example, by a skilled PD physiotherapist), who can also provide expert guidance during their search for the most appropriate strategies. To this end, a variety of strategies should be systematically evaluated in a trial-and-error manner, to identify which suit the patient’s unique situation and needs best. However, a study in 320 Dutch physiotherapists and other PD healthcare professionals revealed that 87% did not use such systematic approach, reportedly due to limited knowledge and skills on the topic [4].
Here, we present a straightforward, practical guide specifically focused on the evaluation of compensation strategies for gait impairment in PD, in support of complementary pharmacological treatments and other elements of physiotherapy [5]. Using this step-wise approach - based on scientific evidence as well as our personal clinical expertise on the topic - we aim to provide healthcare professionals with the tools to evaluate the broad variety of compensation strategies in a systematic, tailored and achievable manner.
1. WHAT ELEMENT OF GAIT IS THE PRIMARY TARGET?
First, determine your primary gait target—of course, there may be multiple targets within one patient in order to optimize functional mobility. Different strategies likely affect different spatiotemporal gait parameters. For example, due to the nature of the cues, auditory cueing (e.g., using a metronome) likely targets stride time, whereas visual cueing (e.g., stepping over lines) targets stride length [6]. Therefore, depending on the primary gait target you and your patient wish to improve (e.g., alleviating episodes of freezing or festination, improving gait rhythmicity, increasing step length, increasing gait speed, improving posture, improving gait initiation) the choice of the most appropriate strategies varies. With progressing disease, the primary target(s) may shift due to increased disability or cognitive decline, which is why—ideally—strategies should be reevaluated periodically.
2. IN WHAT CONTEXT WILL THE STRATEGY BE APPLIED IN DAILY LIFE?
Next, evaluate a strategy’s efficacy in the context in which it will most likely be applied in daily life. This is important because the efficacy of the strategies tends to vary depending on the context in which they are used [3]. The context could entail a certain environment (e.g., what works in the consulting room does not necessarily translate to a crowded marketplace), or a specific situation (e.g., involving an element of time-pressure, or during dual-tasks such as talking while walking). To this end, if possible, it is especially helpful to arrange a home visit to make an inventory of problems that need to be addressed. Perhaps a specifically problematic turn in the kitchen could be tackled by taping down lines on the floor to prevent the occurrence of freezing [7]. If home visits are unfeasible, you could ask your patient to bring a videotape of their home environment to the consultation, or even videotape themselves in the specific areas or situations in which they experience most difficulties.
3. DOES YOUR PATIENT HAVE ANY SPECIFIC PERSONAL PREFERENCES?
Lastly, it is important to consider your patient’s personal preferences. While wearing laser shoes or adopting a new walking pattern may be highly effective, some patients will prefer strategies that are not noticeable to bystanders, avoiding stigmatization or feelings of embarrassment [8]. In these cases, the search for appropriate strategies could be narrowed down to strategies like internal cueing, altering the mental state, action observation and motor imagery. Persons who like to walk alone will probably not be helped by applying action observation, and people who are hesitant to wear headphones in public (e.g., in traffic) will probably not want to use a metronome when walking outdoors. Importantly, you should consider your patient’s cognitive status and learnability, which may largely influence the feasibility of certain compensation strategies. In other words, besides being effective, a strategy should also be usable in daily life according to the intended user: your patient.
Another way to incorporate your patient’s preferences is by making use of their skills or hobbies. If they love music, try walking to their favorite tune over using a metronome. If they are, or used to be, an avid ice skater, have them try making skating motions instead of adopting their usual walking pattern. The search for appropriate strategies is truly a collaborative effort between you and your patient.
HOW TO EDUCATE YOURSELF AND YOUR PATIENTS ON COMPENSATION STRATEGIES
Compensation strategies are often spontaneously ‘invented’ by persons with PD themselves. Consequently, many new strategies do not reach healthcare professionals or other patients, even though additional resources on the available strategies are in high demand. To meet this demand, we have developed a dedicated online platform (https://www.walkingwith parkinson.com) with information on compensation strategies, where patients and professionals can also inspire and learn from each other by sharing videos of their own strategies. The platform is currently available in English and Dutch.
ACKNOWLEDGMENTS
Jorik Nonnekes was supported by a ZonMW Veni grant (16.196.022). The Center of Expertise for Parkinson & Movement Disorders was supported by a center of excellence grant awarded by the Parkinson Foundation.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
REFERENCES
[1] Mirelman A, Bonato P, Camicioli R, Ellis TD, Giladi N, Hamilton JL, Hass CJ, Hausdorff JM, Pelosin E, Almeida QJ (2019) Gait impairments in Parkinson’s disease. Lancet Neurol 18, 697-708.
[2] Nonnekes J, Ruˇzicka E, Nieuwboer A, Hallett M, Fasano A, Bloem BR (2019) Compensation strategies for gait impairments in Parkinson disease: A review. JAMA Neurol 76,718-725.
[3] Tosserams A, Wit L, Sturkenboom IHWM, Nijkrake MJ, Bloem BR, Nonnekes J (2021) Perception and use of compensation strategies for gait impairment by persons with Parkinson disease. Neurology 97, e1404-e1412.
[4] Tosserams A, Nijkrake MJ, Sturkenboom IHWM, Bloem BR, Nonnekes J (2020) Perceptions of compensation strategies for gait impairments in Parkinson’s disease: A survey among 320 healthcare professionals. J Parkinsons Dis 10, 1775-1778.
[5] Gilat M, Ginis P, Zoetewei D, De Vleeschhauwer J, Hulzinga F, D’Cruz N, Nieuwboer A (2021) A systematic review on exercise and training based interventions for freezing of gait in Parkinson’s disease. NPJ Parkinsons Dis 7, 81.
[6] Suteerawattananon M, Morris GS, Etnyre BR, Jankovic J, Protas EJ (2004) Effects of visual and auditory cues on gait in individuals with Parkinson’s disease. J Neurol Sci 219, 63-69.
[7] Tosserams A, de Vries NM, Bloem BR, Nonnekes J (2020) Multidisciplinary care to optimize functional mobility in Parkinson disease. Clin Geriatr Med 36, 159-172.
[8] Maffoni M, Giardini A, Pierobon A, Ferrazzoli D, Frazzitta G (2017) Stigma experienced by Parkinson’s disease patients: A descriptive review of qualitative studies. Parkinsons Dis 2017, 7203259.
-----------
Read the full article published in the Journal of Parkinson’s Disease here:
A Practical Guide to the Evaluation of Compensation Strategies for Gait Impairment in Parkinson’s Disease, by Anouk Tosserams and Jorik Nonnekes, J Parkinsons Dis, vol. 12, no. 6, pp. 2005-2008, 2022, DOI: 10.3233/JPD-223296







- Comment
|